ANTERIOR MINIMALLY INVASIVE TOTAL HIP REPLACEMENT
Anterior Minimally Invasive Surgery in Total Hip Replacement (AMIS) is the state of the art in hip replacement in major hip centers around the world.
Our approach to Total Hip Replacement places equal importance on:
- Optimizing Function
- Maximizing Survivorship
- Accelerating Recovery
Our preferred operative approach is the AMIS technique (Anterior Minimally Invasive Surgery in Total Hip Replacement. It is a commendable technique and its notable advantages over other conventional approaches may be summarized as follows:
- The location of the skin incision in the AMIS technique is such that no nerve or artery are at significant risk of injury.
- The surgical approach exploits an ‘internervous’ interval to reach the capsule of the hip joint. Furthermore, as there is no division of muscle involved in this approach, the approach is not only ’internervous’ but also ‘intermuscular’. It is truly minimally invasive. No tendons or muscles are cut or detached. There is a significant reduction in postoperative pain and stiffness. This makes for greater patient compliance during postoperative physiotherapy. In fact, some of the more physically able patients will recover a ‘normal’ hip feeling in a very short period of time, so much that they must be cautioned not to do too much too soon.
- Although very small in size (6 to 8 cm), the skin incision, due to its position and the trajectory of the deeper dissection, allows for a generous exposure of the femoral neck and head prior to implant insertion.
- The vast majority of our patient population do not require blood transfusion.
- No drain is kept in the surgical wound.
- Hip precautions in the postoperative period can be reduced to a minimum as the rate of dislocation appears to be, in our series as well as in others, next to nil.
- Our results and other results from centers around the world show that hospitalization time, pain, blood loss and work incapacity can be cut approximately in half comparing it with a standard lateral approach.
- Our experience show that the method we use allows us to operate reliably on virtually any patient who needs a hip replacement.
Word of caution
Any patient who needs a Total Hip Replacement should know that Anterior Minimally Invasive Hip Replacement is not a procedure that every surgeon in general orthopedic practice should be doing. The technique is elaborate and the learning curve is long.
I would remain reluctant to determine the number of procedures needed to overcome this so-called ’learning curve’ and I have no doubt this number is not the same for all learners. But at the same time, we believe that a surgeon should not get the experience at the expense of his patients. If the learning curve for an experienced hip surgeon is 40 to 50 Anterior Minimally Invasive Hip Replacement procedures, it is clear that this procedure does not belong to the core pratice of community surgeons who perform hip replacement occasionally.
Many surgeons get the opportunity to travel to a highly specialized center for a one-day training session on using the technique. One day of training is not adequate and we would like to see more extensive ‘hands-on’ cadaver training and mentoring of inexperienced surgeons by those who are skilled in the procedure.

THE ADVANTAGES OF FEMORAL NECK RETENTION IN TOTAL HIP REPLACEMENT WITH “SHORT STEMS”
If you need a hip replacement and your femoral bone is of good quality every effort should be made to retain native bone rather than sacrifice it. This concept is called de-escalation. Retaining the femoral neck when using collum and partial collum short stems potentially improves biomechanical reconstruction and prevents unnecessary dissection to expose the proximal femur, in keeping with the spirit of minimally invasive techniques. (Fig. 1)

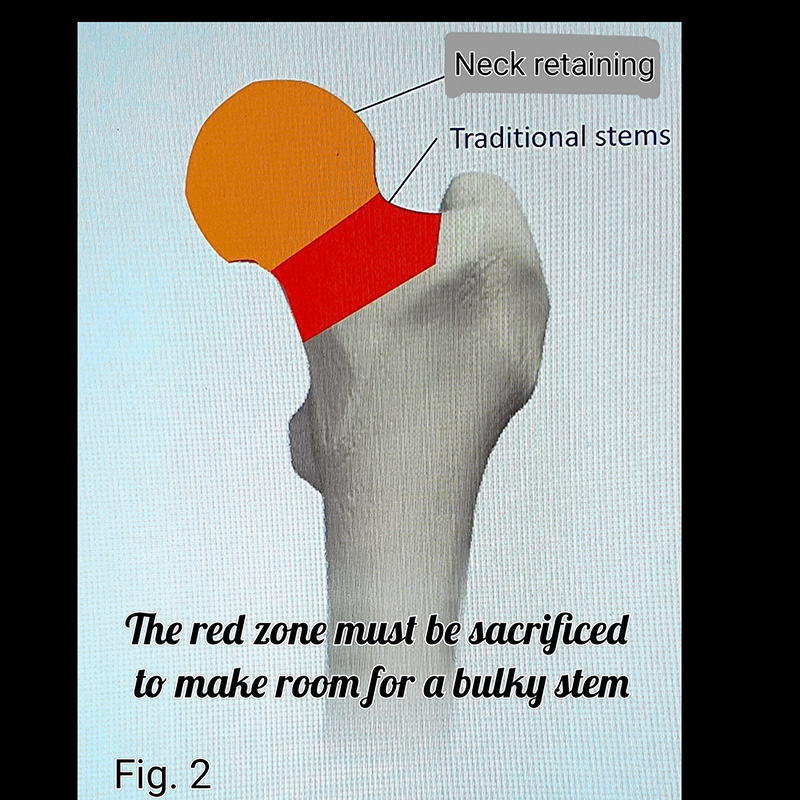
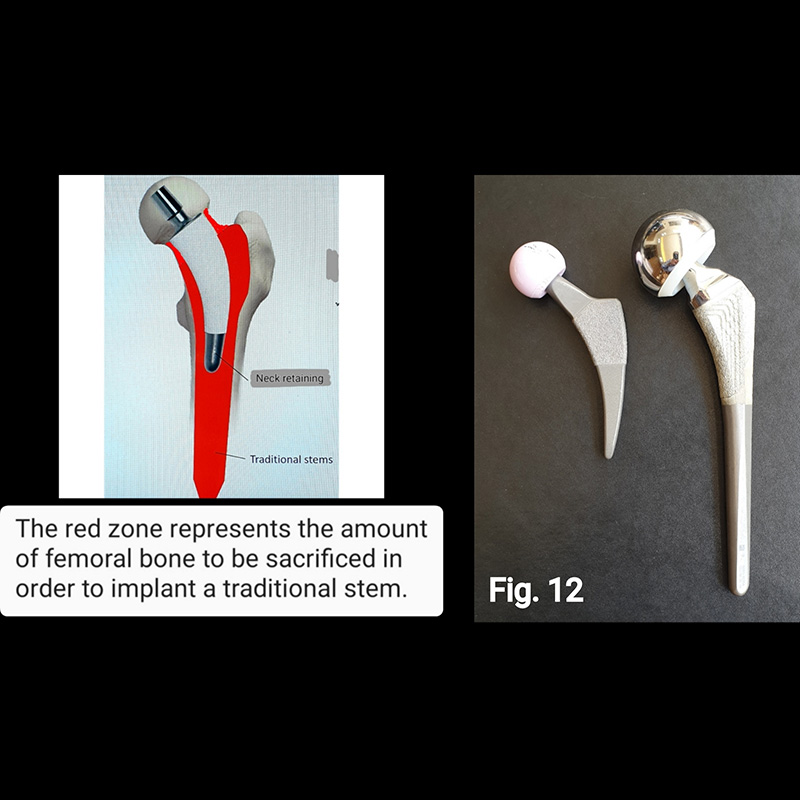
Healthy bone should not be resected for the sole purpose of providing sufficient space for a voluminous implant. (Fig. 2)
The common practice of adapting the patient to the implant is wrong.
In total hip replacement, it is still common practice to resect the head and neck of the femur. This is wrong. The femoral neck is not a throwaway bone, and its preservation is mechanically useful, therefore the question arises, why resect it? There appear to be two arguments for resection, and both arguments are relics surviving from an earlier time in the evolution of orthopedic surgery :
1 – Historical convention: The first prostheses for the replacement of the femoral head were designed for patients with femoral neck fractures where much of the neck was already lost and the idea was to replace the head with a metallic stem passed into the femoral shaft.
2 – Surgical convenience: The femoral neck is an obstacle to inserting a bulky device into the femoral canal. The insertion of the stem into the canal through the resected neck became easier the more bone you remove from the proximal femoral segment. (Fig. 3)

The common practice of adapting the bone to the implant should be abandoned and every effort should be made to adapt the implant to the bone. (Fig. 4)

Implants which respect the existing morphological conditions of the bone appear to give the bone less “work” to achieve integration.
Finite element analysis revealed that load transfer to the proximal femur is more physiological with a femoral neck retaining stem compared to a traditional neck sacrificing stem. Femoral stress distribution with a neck retaining stem has a similar pattern to that of the underanged femur. (Fig.5)
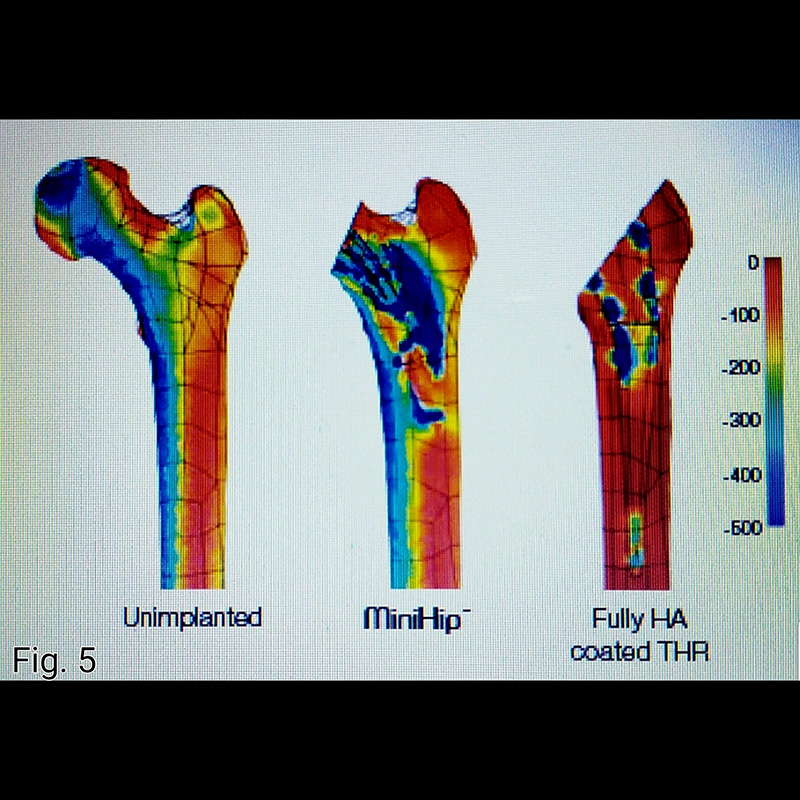
This physiological stress distribution is essential to restore biomechanical equilibrium of the hip.
Optimal anatomy restoration combined with a muscles preserving approach will result in a balanced hip, leading to a forgotten hip perception. The emerging Forgotten Joint Score (FJS) has been suggested to assess patient satisfaction as a more discriminating option compared to traditional scoring systems.
Today’s patients are of a younger age and have a longer life expectancy. They also have higher expectations on their postoperative activity levels. Implants needs therefore to respond to more demanding requisites.
Short-stemmed femoral implants are currently used for total hip replacement in young and active patients to conserve bone, provide physiological loading, restore 3D hip geometry, and reduce the incidence of postoperative thigh pain. For some designs, clinical data collected from large patient cohorts showed a survivorship comparable to traditional stems.
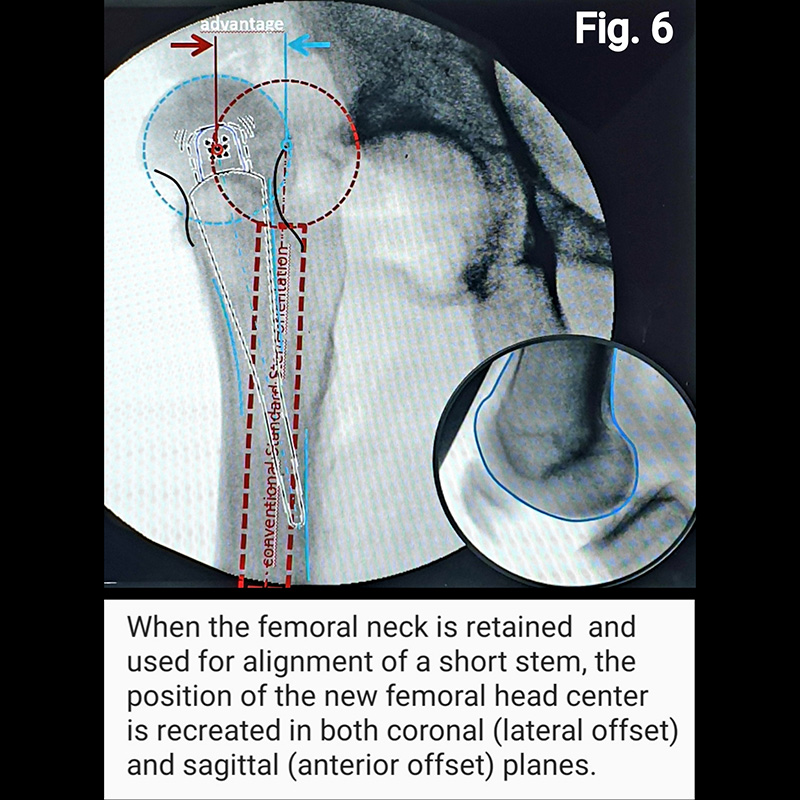
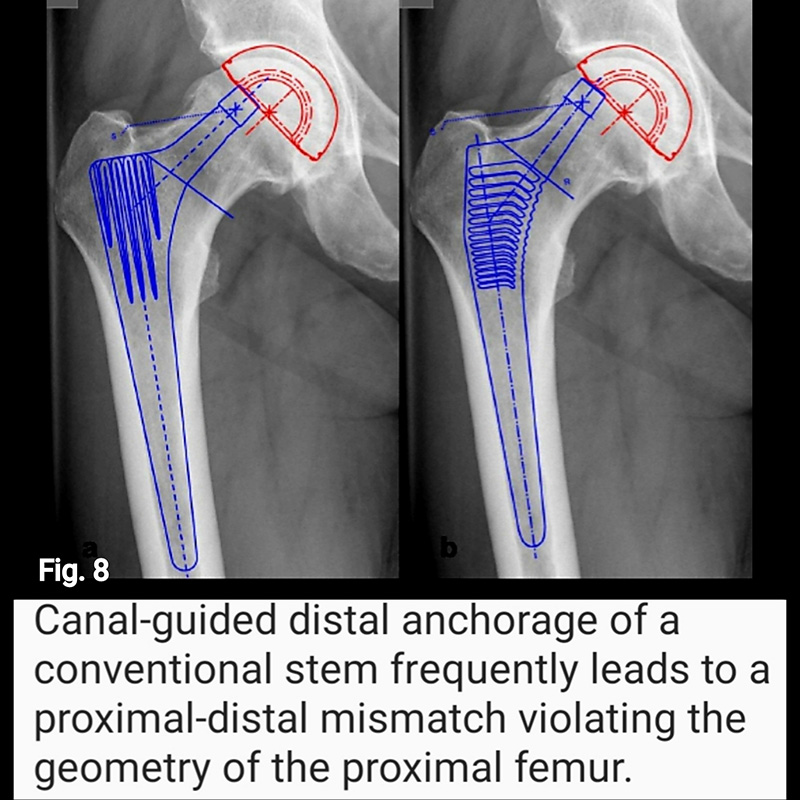
Short stems offer numerous advantages. First, with some short stem designs, a majority of the femoral neck is preserved. Surgically, this requires less surgical dissection and mitigates soft tissue and bone damage. Retaining the femoral neck has significant mechanical advantage in reducing both axial and torsional loads, as well as restoring the center of rotation of the femoral head in the sagittal plane (respect the anterior offset) improving hip balance (Fig. 6), and in the coronal plane (respect horizontal offset) improving abductor strength (Fig. 7 and Fig. 8). Ultimately, preservation of the femoral neck provides a more natural barrier to migration of particulate debris, is associated with less blood loss and less time and energy to rehabilitate the hip, reduces stress shielding of the proximal femur (i.e., load redistribution and subsequent loss of proximal femoral bone mass) (Fig. 9), and reduces end-of-stem thigh pain (spot weld Fig.9).
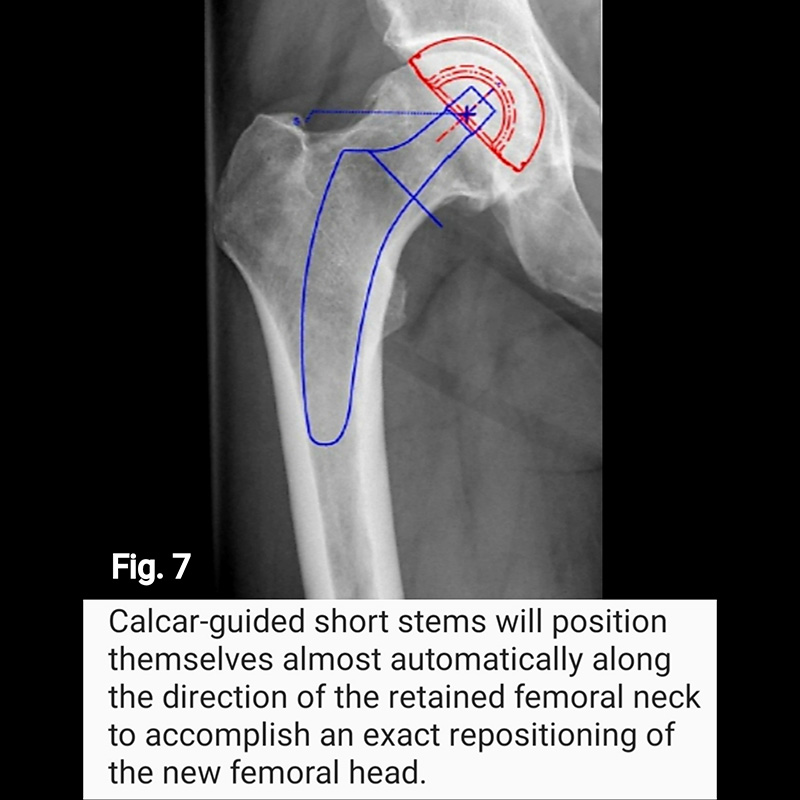

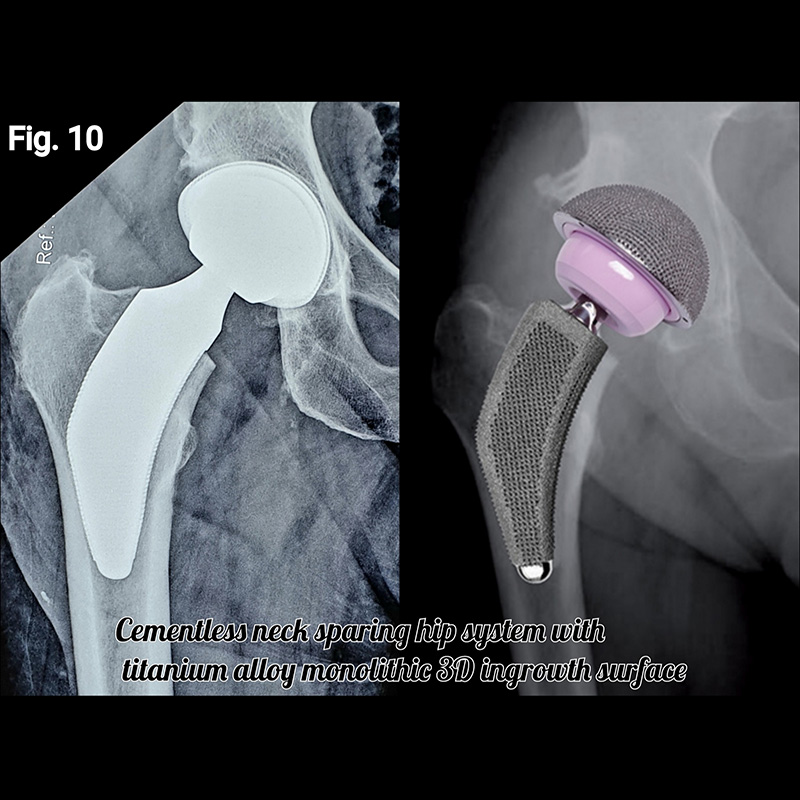
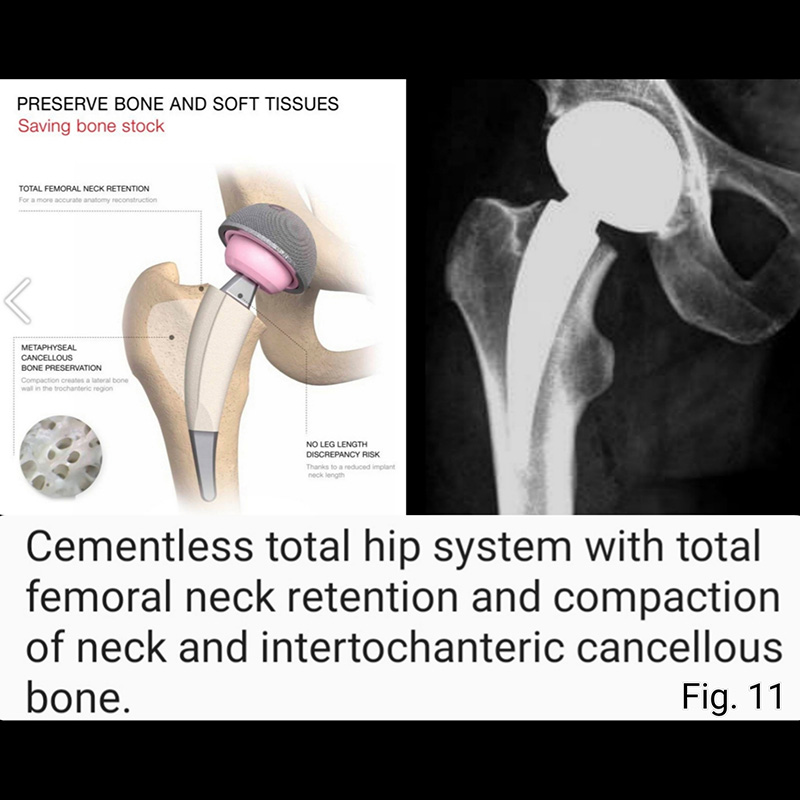
In consideration of all these aforementioned advantages, the use of a short stem can make patient rehabilitation faster and less painful. Because of its smaller size, the short stem is easier to insert, and this facilitates a more minimally invasive surgical approach (Fig. 10 and Fig 11). The novel design feature inherent in short stem implants, namely, preservation of proximal native bone and tissue, theoretically affords easier revision surgery if or when it becomes necessary (Fig.12).
Virtually, every major implant company now offer a “short stem” and now there are a plethora of different designs. It is important to note, however, that not all short stems achieve initial fixation at the same bone interface region, and the surgeon must be aware of the surgical preparation difference for a short metaphyseal style stem versus a neck preserving style stem.
The short neck-stabilized stems and metaphyseal-stabilized stems have demonstrated excellent clinical results. Improved bone remodeling has been impressive. We are encouraged with our experience with short stems which has exceeded 10 years and we continue to use and evaluate these devices.
HIP RESURFACING
Unlike Total Hip Replacement (THR), which requires the removal of the top of the femur and insertion of a stem into the bone shaft, Hip Resurfacing puts a metal ‘cap’ over a reshaped femoral head, thus saving both the head and neck and eliminating the need to enter the intramedullary canal.
Proponents point to these benefits, as well as to the greater stability and decreased risk of dislocation due to the larger femoral head size, as reasons for surgeons to choose resurfacing rather than replacement.
Critics caution, however, that the procedure is far more difficult to perform than THR, that few patients meet the criteria for surgery, and that increased risk of femoral neck fracture and an unknown potential for metal-on-metal ion toxicity exist.
Hip Resurfacing is not a procedure that every surgeon in general orthopaedic practice should be doing. The learning curve is long and patient selection is important to the success of the procedure. Hip Resurfacing has a narrow focus. In a hip replacement service, maybe less than 10 % of the patients are absolute indications for resurfacing. The best patients are male less than 55 years old with osteoarthritis and those who have good quality bone stock with a large head/neck ratio.
Hip Resurfacing is a bone stock preservation procedure, especially on the femoral side where only the pathologic bone is removed during reshaping of the femoral head. The ease of revision surgery makes revision of the femoral component comparable to a primary hip replacement.
REVISION TOTAL HIP REPLACEMENT
Joint replacement surgery is undoubtedly one of the greatest medical advances of our time. Hip and knee replacements have been performed in millions of patients worldwide. These procedures have improved patients’ quality of life by easing pain, improving range of motion, and increasing activity levels.
Although joint replacement surgery has been amazingly successful, approximately ten percent of implants will fail over time and require a second procedure, called revision, to remove the old implants and replace them with new components.
Joint revision surgery is a complex procedure that requires extensive preoperative planning, specialized implants and tools, and mastery of difficult surgical techniques to achieve a good result.
Most hip and knee replacement procedures will perform well for the remainder of the patient’s life. Current hip and knee replacements are expected to function at least 10 to 20 years in 90 percent of patients. This is due to several factors.
- There are more surgeries performed on older individuals. Older individuals tend to put lower demands on their implants.
- Current state-of-the-art materials and techniques have improved the quality of implant fixation to bone. This had historically been a weak link that created a potential site of failure.
- Innovations in implants technology. Innovations have significantly decreased the amount of wear particles that are created by friction on joint surfaces.
- Concentration of expertise. The best results are achieved by the subspecialized surgeon working in a standardized surgical environment.
As increasing numbers of young patients have these procedures, and as seniors continue to live longer, a growing segment of joint replacement patients will outlast their implants.
The decision to perform a revision joint replacement surgery will be based on several factors. The joint may become painful or swollen, due to loosening, wear or infection. The function of the implant may decline, resulting in a limp, stiffness, or instability. Finally, serial examinations or X-rays may demonstrate a change in the position or condition of the components. All of these factors will determine when joint revision surgery is needed.
REASONS IMPLANTS MAY FAIL
The anatomy of the hip and knee is very different after joint replacement as compared with its preoperative state. For example, there are large metallic objects and possibly cement.
In addition there may be scar tissue and bone loss. These factors must be addressed in revision joint surgery.
Implants may fail for any of several physiologic reasons: loosening, infection, dislocation, or patient-related factors. The anatomy and pathophysiology of failed joint replacement implants contribute to the decision to perform revision surgery.
Loosening
Some revisions will be necessary because the implants have loosened . When they were first put in, the large metal and plastic implants of joint replacement were placed with the intention of staying fixed for a long time. They were either cemented into position or bone was expected to grow into the surface of the implant. In either case, the implant was firmly fixed to bone.
However, the friction of the joint surfaces rubbing against each other wears away the surfaces of the implant, creating tiny particles. These particles accumulate around the joint. In a process called aseptic, or noninfected, loosening, the bonds of the implant to the bone are destroyed by the body’s attempts to digest the wear particles. When the prosthesis becomes loose, the patient may experience pain, deformity, or instability. In addition, the process of digestion, or lysis, of wear particles also digests normal bone. This can weaken or even fracture the bone, and jeopardize the success of the revision surgery. In this event, surgery will also address the bone stock deficiencies. Aseptic loosening is the most common mode of failure of hip and knee implants.
Infection
Infection is another physiologic cause of implant failure. The large foreign metal and plastic implants can serve as a surface for bacteria to latch onto. In addition, the tissue that has been previously operated on has an altered blood supply, which may not be adequate to fight infection. Even if the implants remain well-fixed, the pain, swelling, and drainage often make revision necessary. Lastly, the chronic fight against an infection can weaken the patient and endanger their life. Realistic risk of infection with current surgical techniques and antibiotic regimens is about 0.5%.
Dislocation
Dislocation is yet another mode of failure of joint replacement surgery. (Dislocation is a sudden popping out or migration of the implant from its normal position). It is more commonly a problem of hips rather than knees. The rate of dislocation after hip replacement ranges from zero to 10%, but averages about one in 50 patients. Some of these patients will experience multiple dislocations and require revision. The dislocation may be caused by loosening, inadequate soft tissues, bony or scar tissue impingement, incompatible component position, neurologic factors (such as neuropathy or Parkinsonism), or patient noncompliance.
Patient-Related Factors
Younger and more active patients have a higher rate of revision. Obese patients have a higher incidence of wear and loosening .
Patients whose primary surgery was performed for inflammatory arthritis, patients with avascular necrosis, and patients with a previous hip fracture are at higher risk for loosening. These anatomic and physiologic conditions lead to the necessity of joint revision surgery.
DIAGNOSIS
Joint replacement surgery has been shown to decrease pain and increase function in the vast majority of patients. Once a patient progresses through the postoperative period, symptoms of pain, as well as the stability and motion of the joint, should remain stable for an extended period of time.
The natural history of failed implant surgery is an increase in pain, a change in the position of the implant, or a decrease in the function of the implant with limp or dislocation. Patients who demonstrate these symptoms and signs may require revision joint surgery. Therefore, a standard assessment is performed, including a history and physical examination, X-rays, laboratory tests, and possibly aspiration or scintigraphic studies.
SURGICAL INTERVENTION AND CONSIDERATIONS: HIP SURGERY
Greater than 90% of patients who undergo revision procedures will be expected to have good to excellent results, even considering the higher rate of complications as compared to first-time joint replacement. After weighing the alternatives, most patients and physicians prefer revision to other surgical options.
Surgical intervention with joint replacement surgery can be a complex and challenging procedure. Several potentially difficult portions of the surgery must be considered. Common to all joint revisions is an assessment of existing bone quality, removal of failed components, reconstruction of remaining bone and soft-tissue structures, and successfully fixing the new components to the bone.
Consideration of each of these challenges is essential to produce successful revision joint surgery.
In hip revision surgery, both the femoral (stem and ball) components as well as the acetabular (socket) portion must be addressed.
- The hip bones may have deficiencies due to lysis and loosening, fracture, or shielding of the bone from normal stress. These deficiencies are graded according to several classification methods.
- Once this assessment is performed, a method to remove the existing components is selected. If some parts of the implant are still functioning, efforts may be made to retain them. Specialized removal techniques have been developed, including surgically splitting the femur bone to remove the cement and implants, as well as power and hand instruments, which accurately cut around the prosthesis.
- When the failed components are removed, the remaining bone may require a complex reconstruction, involving larger or longer implants, bone grafting using ground-up bone or large segments of bone, and possibly special purpose implants like metal cages, pedestal cups and trabecular metal wedges.
- Finally, the selected revision hip implant must be firmly fixed to the bone, either through bone growing into small pores in the outer layer of the implant or by cementing the construct into place. In our service we prefer the former technique. We do not use cement to fix an implant to bone in hip replacement, be it primary or revision surgery.
POTENTIAL SURGICAL COMPLICATIONS
Any surgery can have potential complications. The complexity of revision joint surgery increases the chance of complications. A realistic assessment of these risks is essential prior to a revision procedure.
Infection, bleeding, and trauma to nerves or blood vessels are a potential with any surgical procedure. These are addressed and minimized by using antibiotics before and after surgery, working in a sterile operating room, use of blood-preserving techniques, and utilizing well-planned surgical exposures. The risk of these complications is higher than primary procedures.
Malpositioning or loosening of the new components is possible. In addition, the revision implants may migrate due to poor bone quality or inadequate fixation to the bone. More severe destructive processes with greater preoperative bone loss are more likely to create this problem.
Deep venous thrombosis and pulmonary embolism, or blood clots in the legs or lungs, can occur in conjunction with a revision procedure. The extensive surgery with subsequent twisting and trauma of the blood vessels can create clotting. In addition, the relative immobility of the patient after surgery increases the chance of clots. A clot in the lungs can become a life-threatening situation if the clot is large.
Dislocation of a hip implant is more common after revision surgery. This is due to the extensive dissection required to remove the failed components as well as the poorer quality of the surrounding soft tissues after multiple procedures. In order to decrease the chance of dislocation, soft tissues are stretched out, which can lead to a lengthening of the operated leg.
Medical conditions can be aggravated or caused by the extensive revision procedure. Patients may have heart and lung complications, or stroke conditions. Rarely, death can occur. The decision to perform revision joint surgery is made when benefits of pain relief and functional improvement outweigh the risk of these potential complications.
CONCLUSION
The decision to have joint revision surgery is based on many factors. Although joint replacement is successful in many patients, certain signs and symptoms will indicate that the implant has failed. Joint revision surgery is necessary when pain, swelling, limp, stiffness, or instability of a failed prosthesis become too great. Fortunately, modern techniques and materials for revision surgery will yield many more active years for most patients.
HIP OSTEOPLASTY FOR FEMOROACETABULAR IMPINGEMENT
Femoracetabular Impingement (FAI) or hip impingement syndrome is a condition affecting the hip joint in young and middle-aged adults. The bones of the hip are abnormally shaped. Because they do not fit together perfectly, the hip bones rub against each other and cause damage to the joint.
Anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, low friction surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket, creating a tight seal and helping to provide stability to the joint.
Description
In FAI, bone spurs develop around the femoral head and/or along the acetabulum. The bone overgrowth causes the hip bones to hit against each other, rather than to move smoothly. Over time, this can result in the tearing of the labrum and breakdown of articular cartilage (osteoarthritis).
There are three types of FAI: pincer, cam and combined impingement.
Pincer. This type of impingement occurs because extra bone extends out over the normal rim of the acetabulum. The labrum can be crushed under the prominent rim of the acetabulum.
Cam. In cam impingement the femoral head is not round and cannot rotate smoothly inside the acetabulum. A bump forms on the edge of the femoral head that grinds the cartilage inside the acetabulum.
Combined. Combined impingement just means that both the pincer and cam types are present.
How FAI progresses. It is not known how many people may have FAI. Some people may live long, active lives with FAI and never have problems. When symptoms develop, however, it usually indicates that there is damage to the cartilage or labrum and the disease is likely to progress. Symptoms may include pain, stiffness and limping.
Cause
FAI occurs because the hip bones do not form normally during the childhood growing years. It is the deformity of a cam bone spur, pincer bone spur, or both, that leads to joint damage and pain. When the hip bones are shaped abnormally, there is little that can be done to prevent FAI.
Because athletically active people may work the hip joint more vigorously, they may begin to experience pain earlier than those who are less active. However, exercise does not cause FAI.
Symptoms
People with FAI usually have pain in the groin area, although the pain sometimes may be more toward the outside of the hip. Sharp stabbing pain may occur with turning, twisting and squatting, but sometimes, it is just a dull ache.
CEMENTLESS TOTAL KNEE REPLACEMENT
At the end of a lecture I gave a few years ago during an orthopaedic seminar, advocating cementless knee replacement to an audience divided between proponents and critics, a question was addressed to Professor Chitranjan Ranawat, a world authority in knee replacement at the Hospital for Special Surgery in New York who was present in the group and leading the discussion, asking his opinion about the future of knee replacement. Professor Ranawat was very clear, I quote him: “Ten years from now, all total knee replacements will be cementless”.
His vision would appear even more realistic if we look back at the evolution of total hip replacement. Cemented total hip replacement was the golden standard in the 1980s when cementless total hip replacement was only the exception. In just two decades the trend has reversed such as we reached today a market dominated by cementless total hip replacement. I can see no reason why we should not witness a similar shift in total knee replacement in the not too distant future.
The application of a layer of cement to fix an implant to bone means the interposition of an inert interface between the implant and the bone. This interface is at its prime on the day it is applied. It can only deteriorate with the passage of time.
A cementless implant bonds directly, under coaxial pressure, to a matching reshaped bone surface, a technique called ‘press-fit’ thus, achieving ‘primary stability’ of the implant. Primary stability allows immediate full weight bearing ambulation of the patient.
The back of a cementless implant, that is the surface coming into direct contact with bone, is manufactured from bone-friendly material capable to invite bone growth into it and around it, resulting in a strong and viable biological bond between implant and bone which will get stronger with the passage of time. This is called ‘secondary stability’.
Primary stability and secondary stability in cementless total knee replacement can be achieved with precision instrumentation and advanced surgical engineering,
Cementless Total Knee Replacement is technically less forgiving than cemented total knee replacement, in a sense that minor imperfections in bone cutting with consequent bone-implant mismatch can be hidden with cement.
Therefore, Cementless Total Knee Replacement is surgeon sensitive (experience). And to a lesser extent, it is also patient sensitive ( bone stock quality) and prosthesis sensitive (not all implants are the same).
We like to match our Cementless Total Knee Replacement to a rotating platform design (mobile bearing) thus dissociating flexion from rotation.
In fixed bearing knee designs, flexion and rotation occur in the same plane between the femoral component and the polyethylene insert, leading to multidirectional polyethylene wear.
In mobile bearing designs (rotating platform), flexion and rotation occur in separate planes. Flexion occurs between the femoral component and the polyethylene insert, while rotation occurs at a lower level between the polyethylene insert and the tibial component, leading to monodirectional polyethylene wear either in flexion or in rotation.
It has been demonstrated that monodirectional wear is less important than multidirectional wear, therefore a mobile bearing knee will potentially improve survivorship.
Therefore, in an effort to improve postoperative function, reduce surgical time and maximize survivorship we have selected a state of the art total knee prosthesis featuring:
- cementless implantation
- rotating platform
- anteroposterior stabilization
- patella-friendly trochlear groove
- improved interaction of the posterior femoral condyles on the articular surface
We started Cementless Total Knee Replacement in 2004 with excellent results and consistent high score patient satisfaction, implanting a knee prosthesis suitable for the vast majority of patients requiring knee replacing, including the younger patient with higher athletic aspirations.
With its cutting-edge design matched to a meticulous surgical technique paying attention to the finest details, our Cementless Total Knee Replacement is best appreciated with patients capable of higher flexion to optimize its benefits, such as those whose cultural customs or work activities require deep flexion.
Currently, our indications for cemented knee replacement are limited to the geriatric population with limited physical expectations, when the extra cost for a cementless prosthesis is not justified.
UNICOMPARTMENTAL KNEE REPLACEMENT
Unicompartmental knee replacement is an option for a small percentage of patients with osteoarthritis of the knee. Your doctor may recommend partial knee replacement if your arthritis is confined to a single part (compartment) of your knee.
Your knee is divided into three major compartments: the medial compartment (the inside part of the knee), the lateral compartment (the outside part) and the patellofemoral compartment (the front of the knee between the kneecap and thighbone).
In a unicompartmental knee replacement, only the damaged compartment is replaced with metal and plastic. The healthy cartilage and bone in the rest of the knee is left alone.
Advantages of Partial Knee Replacement
Multiple studies have shown that modern unicompartmental knee replacement performs very well in the vast majority of patients who are appropriate candidates.
The advantages of partial knee replacement over total knee replacement include:
- Quicker recovery
- Less pain after surgery
- Less blood loss
Also, because the bone, cartilage and ligaments in the healthy parts of the knee are kept, most patients report that a unicompartmental knee replacement feels more “natural” than a total knee replacement. A unicompartmental knee may also bend better.
In order to be a candidate for this procedure, your arthritis must be limited to one compartment of your knee and you must have exhausted the nonsurgical treatment options.
Patients with inflammatory arthritis, significant knee stiffness, or ligament damage may not be ideal candidates.
Your surgeon will help you determine if this procedure is suited for you. With proper patient selection, modern unicompartmental knee replacements have demonstrated excellent medium and long term results in both younger and older patients.
REVISION TOTAL KNEE REPLACEMENT
Joint replacement surgery is undoubtedly one of the greatest medical advances of our time. Hip and knee replacements have been performed in millions of patients worldwide. These procedures have improved patients’ quality of life by easing pain, improving range of motion, and increasing activity levels.
Although joint replacement surgery has been amazingly successful, approximately ten percent of implants will fail over time and require a second procedure, called revision, to remove the old implants and replace them with new components.
Joint revision surgery is a complex procedure that requires extensive preoperative planning, specialized implants and tools, and mastery of difficult surgical techniques to achieve a good result.
Most hip and knee replacement procedures will perform well for the remainder of the patient’s life. Current hip and knee replacements are expected to function at least 10 to 20 years in 90 percent of patients. This is due to several factors.
- There are more surgeries performed on older individuals. Older individuals tend to put lower demands on their implants.
- Current state-of-the-art materials and techniques have improved the quality of implant fixation to bone. This had historically been a weak link that created a potential site of failure.
- Innovations in implants technology. Innovations have significantly decreased the amount of wear particles that are created by friction on joint surfaces.
- Concentration of expertise. The best results are achieved by the subspecialized surgeon working in a standardized surgical environment.
As increasing numbers of young patients have these procedures, and as seniors continue to live longer, a growing segment of joint replacement patients will outlast their implants.
The decision to perform a revision joint replacement surgery will be based on several factors. The joint may become painful or swollen, due to loosening, wear or infection. The function of the implant may decline, resulting in a limp, stiffness, or instability. Finally, serial examinations or X-rays may demonstrate a change in the position or condition of the components. All of these factors will determine when joint revision surgery is needed.
REASONS IMPLANTS MAY FAIL
The anatomy of the hip and knee is very different after joint replacement as compared with its preoperative state. For example, there are large metallic objects and possibly cement.
In addition there may be scar tissue and bone loss. These factors must be addressed in revision joint surgery.
Implants may fail for any of several physiologic reasons: loosening, infection, dislocation, or patient-related factors. The anatomy and pathophysiology of failed joint replacement implants contribute to the decision to perform revision surgery.
Loosening
Some revisions will be necessary because the implants have loosened . When they were first put in, the large metal and plastic implants of joint replacement were placed with the intention of staying fixed for a long time. They were either cemented into position or bone was expected to grow into the surface of the implant. In either case, the implant was firmly fixed to bone.
However, the friction of the joint surfaces rubbing against each other wears away the surfaces of the implant, creating tiny particles. These particles accumulate around the joint. In a process called aseptic, or noninfected, loosening, the bonds of the implant to the bone are destroyed by the body’s attempts to digest the wear particles. When the prosthesis becomes loose, the patient may experience pain, deformity, or instability. In addition, the process of digestion, or lysis, of wear particles also digests normal bone. This can weaken or even fracture the bone, and jeopardize the success of the revision surgery. In this event, surgery will also address the bone stock deficiencies. Aseptic loosening is the most common mode of failure of hip and knee implants.
Infection
Infection is another physiologic cause of implant failure. The large foreign metal and plastic implants can serve as a surface for bacteria to latch onto. In addition, the tissue that has been previously operated on has an altered blood supply, which may not be adequate to fight infection. Even if the implants remain well-fixed, the pain, swelling, and drainage often make revision necessary. Lastly, the chronic fight against an infection can weaken the patient and endanger their life. Realistic risk of infection with current surgical techniques and antibiotic regimens is about 0.5%.
Dislocation
Dislocation is yet another mode of failure of joint replacement surgery. (Dislocation is a sudden popping out or migration of the implant from its normal position). It is more commonly a problem of hips rather than knees. The rate of dislocation after hip replacement ranges from zero to 10%, but averages about one in 50 patients. Some of these patients will experience multiple dislocations and require revision. The dislocation may be caused by loosening, inadequate soft tissues, bony or scar tissue impingement, incompatible component position, neurologic factors (such as neuropathy or Parkinsonism), or patient noncompliance.
Patient-Related Factors
Younger and more active patients have a higher rate of revision. Obese patients have a higher incidence of wear and loosening .
Patients whose primary surgery was performed for inflammatory arthritis, patients with avascular necrosis, and patients with a previous hip fracture are at higher risk for loosening. These anatomic and physiologic conditions lead to the necessity of joint revision surgery.
DIAGNOSIS
Joint replacement surgery has been shown to decrease pain and increase function in the vast majority of patients. Once a patient progresses through the postoperative period, symptoms of pain, as well as the stability and motion of the joint, should remain stable for an extended period of time.
The natural history of failed implant surgery is an increase in pain, a change in the position of the implant, or a decrease in the function of the implant with limp or dislocation. Patients who demonstrate these symptoms and signs may require revision joint surgery. Therefore, a standard assessment is performed, including a history and physical examination, X-rays, laboratory tests, and possibly aspiration or scintigraphic studies.
SURGICAL INTERVENTION AND CONSIDERATIONS: KNEE SURGERY
Greater than 90% of patients who undergo revision procedures will be expected to have good to excellent results, even considering the higher rate of complications as compared to first-time joint replacement. After weighing the alternatives, most patients and physicians prefer revision to other surgical options.
Knee revision surgery entails consideration of the femur (thigh bone), tibia (shin bone), and patella (kneecap) components.
- Bone stock deficiencies are classified according to several grading systems, and lysis, fracture, or stress shielding can lead to bone loss.
- The failed components are removed by a combination of surgical methods and specialized instruments. Reconstruction may require implants with extensions to reach better-quality bone and that effectively replace lost ligament stability.
- Ground-up or bulk bone graft may be used.
- An implant is fixed in place through cemented or bone in-growth techniques.
POTENTIAL SURGICAL COMPLICATIONS
Any surgery can have potential complications. The complexity of revision joint surgery increases the chance of complications. A realistic assessment of these risks is essential prior to a revision procedure.
Infection, bleeding, and trauma to nerves or blood vessels are a potential with any surgical procedure. These are addressed and minimized by using antibiotics before and after surgery, working in a sterile operating room, use of blood-preserving techniques, and utilizing well-planned surgical exposures. The risk of these complications is higher than primary procedures.
Malpositioning or loosening of the new components is possible. In addition, the revision implants may migrate due to poor bone quality or inadequate fixation to the bone. More severe destructive processes with greater preoperative bone loss are more likely to create this problem.
Deep venous thrombosis and pulmonary embolism, or blood clots in the legs or lungs, can occur in conjunction with a revision procedure. The extensive surgery with subsequent twisting and trauma of the blood vessels can create clotting. In addition, the relative immobility of the patient after surgery increases the chance of clots. A clot in the lungs can become a life-threatening situation if the clot is large.
Medical conditions can be aggravated or caused by the extensive revision procedure. Patients may have heart and lung complications, or stroke conditions. Rarely, death can occur. The decision to perform revision joint surgery is made when benefits of pain relief and functional improvement outweigh the risk of these potential complications.
CONCLUSION
The decision to have joint revision surgery is based on many factors. Although joint replacement is successful in many patients, certain signs and symptoms will indicate that the implant has failed. Joint revision surgery is necessary when pain, swelling, limp, stiffness, or instability of a failed prosthesis become too great. Fortunately, modern techniques and materials for revision surgery will yield many more active years for most patients.
ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION WITH LARS ARTIFICIAL LIGAMENT
Injury to the Anterior Cruciate Ligament (ACL) of the knee is common.
Following complete rupture of the ACL, insufficient revascularization of the ligament prevents it from healing completely, creating a need for reconstruction.
ACL reconstruction aims to reinstate the functional stability of the knee, in turn, preventing further damage to the menisci and reducing the risk of degenerative osteoarthritis. The early success of reconstructive surgery has lead to the progression from open extra-articular stabilization to arthroscopic anatomic grafting
A variety of grafts are available for use in ACL reconstruction. Broadly, all grafts can be placed into one of three categories:
- Autologous grafts
- Allografts
- Synthetic ligaments
Autologous grafts such as hamstring tendons or patellar tendon grafts are widely used. Autologous grafts provide a strong scaffold for ingrowth of collagen fibers without the risk of graft rejection. However, autologous grafts carry a risk of harvest site morbidity and require prolonged avoidance of activities during revascularization for a period up to 12 months.
Allografts (dry of frozen cadaver specimens) are less common and although they eliminate harvest site morbidity, they are prone to graft rejection, potential viral infection risk, slower healing and higher failure rates.
Over the last two decades, with advancing technology, new types of synthetic ligaments have been developed. One of these ligaments the Ligament Advanced Reinforcement System (LARS) has recently gained popularity with some orthopedic surgeons. Dr Omar Baddoura is one of them.
The LARS graft provides a meshwork scaffold for the injured ACL to heal and repair. Unlike traditional ACL reconstruction techniques, the LARS does not require debriding of the torn ACL fibers and synovial lining that normally envelops the ligament. The proposed advantage of this technique is reduced trauma to the soft tissues of the knee and less surgical time. Overall, the LARS surgical technique aims to maximize in-growth of the original ACL tissue, thus preserving some vascular and proprioceptive nerve supply. It is most suited to acute settings where a viable cruciate stump is present.
The potential advantages of LARS are:
- Reduced surgical time
- Eliminate harvest site morbidity
- Immediate graft stability
- Reduced risk of graft breakdown in the early postoperative phase
Due to the LARS potential capacity for early loading it would be inappropriate to stress other types of grafts in the same fashion.
The LARS ACL construct does not need to be protected like autologous grafts in the initial stages, thus eliminating the need to wear a knee brace after the operation.
- Quicker return to pre-injury function. Return to non-competitive sports within 2 months. Return to full pre-injury activity between 3 to 4 months.
- A high patient satisfaction score is a consistent finding.
- With regard to complications arising from LARS, the historical finding of increased reactive synovitis associated with old generations of synthetic grafts, is no longer supported.
KNEE REALIGNMENT PROCEDURES

Osteotomy surgery involves cutting and realigning the bone (usually shin bone/tibia) in order to redistribute the weight going through the knee. In other words, transfer of load from the "sick" to the "healthy" compartment.
Realignment can be achieved by either taking a slice of bone out of the tibia (shin bone) or femur (thigh bone) close to the knee joint (closing wedge) or opening a gap in the bone (opening wedge).
A significant number of patients have isolated damage to one side of the knee whilst the other side of the knee remains healthy. Because most patients are slightly bow-legged it is much more common to wear out the medial (inner) portion of the knee. Here an individual will complain of pain which is predominantly felt on the inner side of the knee. The reverse to this is an individual who is "knock-knees" who is more likely to sustain wear and damage to the outer (lateral) compartment of the knee.
In this country the most commonly carried out procedure for severe wear and tear is a Total Knee Replacement or a Partial Knee Replacement (Unicondylar Knee Replacement). However, there is evidence that young people tend to do less well with a knee replacement than more elderly patients. Where a patient is suitable an osteotomy may represent an excellent alternative to knee replacement surgery.
The key to this procedure is patient selection. Suitability for osteotomy surgery around the knee depends on a number of factors which include age, range of motion, stability, limitation of damage into one compartment. The two most important factors appear to be residual cartilage and extra-articular varus/valgus. Radiological studies of both lower extremities are necessary for assessment and preoperative planning. With a careful patient selection and an appropriate surgical technique the results of osteotomy at 10 years should be superimposable onto those of knee replacement.
CUSTOM-FIT TOTAL KNEE REPLACEMENT
This is a patient matched technology in knee replacement. The core of this technique is a patient-specific cutting block allowing the surgeon to realize his pre-operative 3D planning, based on CT images of the patient’s knee. This innovative concept combines different features giving potential benefits to both the patient and the surgeon:
-
ACCURATE IMPLANT POSTIONING
The cutting blocks are made to accurately match the surgeon’s preoperative planning based on individual patient’s anatomy and his mechanical axis.
Unmistakable positioning of the cutting guides on the bone, referring to distinct references: the osteophytes.
-
NO INTRAMEDULLARY CANAL VIOLATION
- Less bleeding
- Less risk of emboli
- Less transfusions
-
UP TO 60% REDUCTION OF SURGICAL STEPS FOR BONE RESECTION AND RELATED TIME
Only 3 surgical steps are needed using the cutting guides: fit-pin-cut, saving more than 20 steps, significantly reducing the overall surgical time.
Moreover the patient may benefit from:
- Less exposure to the risk of infection
- Less time under anaesthesia
- Less tourniquet time
-
UP TO 60% REDUCTION OF TIME AND COST IN WASHING, ASSEMBLING AND STERILIZATION PROCEDURES
- Only 2 trays opened versus 6 or more for a conventional Total Knee Replacement
- Specific implants ready in the operating room
- Fewer cleaning requirements
- Improved overall operation room logistics and efficiency
-
INTERACTIVE 3D WEB PLANNING
- The preoperative planning is based on the surgeon’s specific preferences and submitted to the surgeon for approval through an interactive website
- For every case the surgeon can modify all femoral and tibial parameters such as femoral distal and anterior-posterior resection levels, femoral rotation, femoral flexion, femoral and tibial varus/valgus, tibial resection level and tibial slope
- Once approved by the surgeon, the cutting blocks are produced using laser sintering technology
- The guides are then shipped to be setup for surgery
BUNION CORRECTION WITH SCARF OSTEOTOMY AND AKIN OSTEOTOMY
Hallux Valgus (Bunion)
What is it?
Hallux Valgus is a deformity of the big toe and forefoot. There is splaying of the first and second metatarsal bones which makes the forefoot wide. The soft tissue attachments to the big toe then pull the big toe towards the smallest toes. As the foot becomes broad the skin rubs on shoes and the skin can be inflamed. This bony lump with its overlaying inflamed skin is a bunion.
What problems does it cause?
The main problem with this condition is pressure over this bony prominence from shoe wear. The skin can sometimes become red and blistered. If the foot is very broad then it may be difficult to get wide enough fitting shoes.
As the big toe moves sideways it can touch the second toe. If the big toe moves further it can lie under the second toe pushing it upwards. The second toe can hence rub on shoes.
In a normal foot the weight is taken under the first metatarsal. In hallux valgus this mechanism may not work as efficiently and the other metatarsals may have to take more weight. This can cause pain under the ball of the foot. This is called metatarsalgia.
Sometimes the joint can wear out, this is called osteoarthritis. This can be painful.
Are bunions hereditary?
Bunions do tend to run in families. However if you have a bunion your children will not necessarily have one too. Bunions are more common in females rather than males.
Are shoes to blame?
Bunions can occur in populations in which shoes are not worn. However, shoes which squeeze the big toe or that do not fit properly may exacerbate the deformity in a patient with a broad forefoot.
What can be done about a bunion?
Most of the difficulty with bunions arises from shoe wear. Many people are comfortable if they wear wide, well fitting shoes. Sometimes the leather needs to stretch and so it is important to allow time for the feet to adapt to new shoes. Sometimes a small pad over the bony prominence can take pressure off the bunion.
High heeled shoes tend to squeeze the foot at the front where the foot is broadest. This can make pressure problems worse.
Some shoes shops can stretch your new shoes with special moulds to make the shoes wider. It is worth asking at the shoe shop or a cobbler.
Can an operation cure a bunion?
If simple measures do not make you comfortable then an operation may improve the situation. The operation should aim at correcting the deformity of your toe and narrowing your foot back towards what it should be. There are many operations to correct bunions depending on the severity of the deformity and the shape of your foot. The vast majority of these operations include an osteotomy. An Osteotomy is a surgical operation whereby a bone is cut to shorten, lengthen, or change its alignment.
The operation involves several procedures designed to narrow the foot and straighten the big toe. It is done through two incisions (cuts), one on the top of the foot between first and second toes and the other one on the inner side of the first metatarsal. A tendon (adductor hallucis) is divided which will help to bring the toe back to normal position. The Scarf osteotomy is performed on the first metatarsal bone. It is my procedure of choice to deal with bunions (Hallux Valgus deformity). Its potential for correction exceeds that of other existing techniques. The word Scarf is a term used in carpentry to describe the notching of two pieces of wood so that they interlock and form a strong bond. This notching technique is the basis of the Scarf osteotomy procedure. Specifically, the long bone, or metatarsal, of the first toe is sliced horizontally and two transverse cuts or notches are made at each end of the bone to complete the osteotomy in a Z shape. The lower piece of the first metatarsal is moved inward to reduce the angle between the first and second metatarsals and bring the toes closer together.
Once the pieces are in their new position, the two sections of the first metatarsal are connected with two small screws. Reducing the angle between the first and second metatarsals also reduces the size of the bunion. Any bone still protruding in the area of the bunion can then be shaved off and given a smooth surface.
In severe cases, an additional osteotomy, the Akin osteotomy, performed on the big toe bone improves the correction. A wedge of bone is removed from the base of the phalynx and the toe is readjusted and straightened. The bone is anchored with a surgical staple.
The capsule of the joint is repaired to keep the toe in straight position.
The patient will have dissolvable stitches.
No plaster is required.
After the operation
- The patient will be on crutches, walking on the heel for 6 weeks, wearing special purpose orthopaedic shoes.
- They will have moderate pain to the scale of 5/10. They will need some pain killers for the first few days and keep the foot elevated until the swelling settles.
- There will be a bulky cotton dressing, which will be changed to a lighter dressing at the first follow-up appointment after 12 days when the wound will be checked.
- The patient will then be followed up in clinic at 6 weeks to assess healing.
- They may need 6 weeks off work depending on the nature of their job.
- The patient won’t be able to drive until they can do an emergency stop without pain in the foot.
Conclusion
The Scarf osteotomy is a powerful and versatile procedure to correct hallux valgus deformity. This allows the patient to ambulate postoperatively early, as the osteotomy is inherently stable, and return to work at an earlier date as compared to other procedures. Bilateral procedures are also possible. Scarf osteotomy provides a predictable and satisfying result. Scarfs are not considered as a single osteotomy but as a combination of several procedures and displacement in several planes are possible. The indication can be extended to severe hallux deformities including secondary deformities as in juvenile and rheumatoid hallux deformity.

A scarf joint in the dining room ceiling of the Fluela Hotel in Davos, Switzerland
RECONSTRUCTION OF LIGAMENTS AND TENDONS WITH LARS ARTIFICIAL LIGAMENT REINFORCEMENT
Repair of Achilles Tendon Rupture with LARS Artificial Ligament Reinforcement
The Achilles Tendon is the most commonly ruptured tendon in the body and yet its management remains controversial due to potential surgical complications.
Patients who undergo traditional repair of their Achilles Tendon take a long time to return to function. The traditional surgery requires prolonged leg immobilization in plaster followed by months of exhaustive physiotherapy. Moreover, the risk of re-rupture will always be present following a conventional repair with or without an autologous graft.
We believe that primary or secondary repair using LARS ligament augmentation, combined with early mobilization will significantly reduce all these potential problems and lead to improve functional outcomes.
The results of our clinical series indicate that LARS ligament repair of acute and chronic Achilles Tendon ruptures provides a reliable and effective technique for repair. It eliminates the need for graft harvesting, it decreases postoperative complications, but most importantly, patients have improved functional outcomes. No postoperative cast immobilization is required and the ankle is mobilized the day after surgery. Patients return to normal life and sporting activities in a relatively short period of time. We have had no cases of re-rupture.
OPERATIVE FRACTURE CARE
With a background of more than two decades of practice at the American University of Beirut Medical Center we have built up a vast experience in the treatment of musculo-skeletal injuries.
Our aim is to offer sophisticated diagnoses and innovative treatments at a leading international level in tandem with high quality service for patients of all ages.
Expertise:
- Adult and pediatric musculo-skeletal injuries of the upper limb
- Adult and pediatric musculo-skeletal injuries of the lower limb
- Fractures of the pelvis and acetabulum
- Minimally Invasive Plate Osteosynthesis (MIPO)
- Repair of nonunions and malunions
- Management of complications and medical negligence